We are aware of incorrect information about AIC’s financial assistance schemes being circulated. Always verify details on our website first. If in doubt, contact AIC directly.
Interim Disability Assistance Programme for the Elderly (IDAPE)
Monthly cash payouts to help older Singaporeans with severe disabilities manage care costs.

Highlights
Introduction
The Interim Disability Assistance Programme for the Elderly (IDAPE) is an assistance scheme set up in 2002 for a small group of seniors. They were not eligible for ElderShield at the time, because they were too old or had pre-existing disabilities.
The monthly payout can be used for long-term care needs, such as hiring a helper, paying for care services, or daily expenses.
How to qualify
There are a few criteria your loved one will need to meet to qualify for IDAPE.
| Criteria | Description |
|---|---|
| Care recipient's nationality and residence | He/ she must be a Singapore Citizen living in Singapore. |
| Care recipient's age |
He/ she must be:
|
| Care recipient's household income |
He/ she must meet the means-test criteria for IDAPE:
OR
|
| Care recipient's needs |
He/ she must:
|
| Care recipient's eligibility for other schemes |
He/ she must:
|
How the scheme works
The amount of payout depends on your monthly household income per person.
| Monthly household income per person | Payout Amount |
Payout Duration |
| $0 – $2,600 (or AV ≤ $21,000 for households without income) |
$250 | Up to 72 months |
| $2,601 – $3,600 | $150 |
After you submit your application, we may take up to four weeks to process it. You will be informed about the outcome in writing via mail.
Once approved, payouts will be made to the nominated bank account in the following month. This may include payouts from the month the application was submitted. The payouts will be reflected as “IDAPE” in your bank statement.
How to apply
There are several ways you can apply for IDAPE.
-
Apply online using Singpass (recommended)
This is done via AIC’s e-Services for Financing Schemes (eFASS). We recommend this method as the approval waiting time is shorter.
Read the terms and conditions before you start.
Please read here if you are applying for the grant on behalf of someone who lacks mental capacity.
-
Seek assistance from the nursing home your loved one is staying in
If you are applying for IDAPE to help you offset the cost of the nursing home fees, you can ask the service provider to help. You can nominate the payout to be made directly to the nursing home.
-
Apply via hard copy
Email apply@aic.sg to obtain a copy of the application form or visit any AIC Link.
We seek your understanding that hardcopy applications take a longer time to process.
Documents needed
The full details of what is needed are available on eFASS.
FAQs
FAQs
Household monthly income per person is the criteria used when there is a household income. (“Household” refers to the NRIC address)
It is calculated as the total gross household monthly income divided by the total number of family members living together in the household. Gross monthly household income includes basic employment income, trade/self-employed income, overtime pay, allowances, cash awards, commissions, and bonuses.
When there is no household income, Annual Value (AV) is used instead. AV is the estimated gross annual rent of a property if it were to be rented out, excluding furnishings and maintenance fees. It is determined by IRAS, and may be checked via IRAS website. Subsidy levels in 2026 will be determined using 2025 Annual Values.
To check or update your household information for means-testing, please use the MediShield Life Household Check e-Service. Alternatively, you can call the Medishield Life Hotline at 1800 222 3399.
He/ she will need to see an MOH-accredited severe disability assessor who will determine their disability level.
There is an assessment fee you will need to pay first, which will be reimbursed if your loved one is assessed to be severely disabled.
If he/ she is found to have mild or moderate disability instead, there are other financial assistance schemes that you can turn to for help, like the Home Caregiving Grant or MDW Levy Concession. Please find out more about the other financial assistance schemes here.
The cost of the assessment ranges from $100 (if you visit the assessor’s clinic) to $250 (if the assessor needs to do a home visit).
You will need to pay the assessment fee first to the assessor. The amount will be reimbursed if your loved one is assessed to be severely disabled.
The assessment must be done by a MOH-accredited severe disability assessor.
He/ she needs to be assessed by an MOH-accredited severe disability assessor.
Please check if your doctor or therapist is on the approved list of assessors. If they are not, please make an appointment with another assessor from the list.
You can apply on behalf of your loved one as long as:
- You are the appointed Donee (appointed under the Lasting Power of Attorney) or Deputy (appointed under the Mental Capacity Act) authorised to make decisions on his/ her property and affairs.
- If your loved one does not have a Donee or Deputy, you can apply on his/ her behalf if you are an immediate family member (parent, spouse or child. Otherwise, you can only apply on his/ her behalf if the immediate family members are unable to do this (eg deceased, lack mental capacity or other issues). For successful applications without a donee/deputy, the caregiver or another family member has 12 months to obtain a court order appointing him/ her as a deputy, failing which the payouts will be suspended. Do visit the Singapore Courts website to find out how to apply for a deputyship.
- You may need the following documents:
-
Recent medical report stating that he/ she lacks mental capacity
OR
Doctor’s certification that he/ she lacks mental capacity
- If the care recipient is also going for a disability assessment, you must ask if the doctor can do a mental capacity assessment (using this form) at the same time.
- The doctor’s certification is valid for six months, unless stated as permanent.
OR
Court order of deputy appointment
- Copy of bank book or statement if the bank account nominated to receive the grant belongs to a deputy or trustee.
-
No, as such conditions affect people’s ability to carry out the six activities of daily living at different levels.
In order to qualify for IDAPE, your loved one still needs to undergo a disability assessment by an MOH-accredited severe disability assessor. The assessor will consider the impact of your loved one’s cognitive challenges as part of the assessment.
This may sometimes be required to confirm if your loved one still meets the qualifying criteria. You will be informed by mail if this is needed. The re-assessment fees are waived regardless of the outcome.
If your loved one has been assessed as permanently severely disabled, he/ she will not need future re-assessments, unless new information suggests that his/ her condition has improved.
Yes, you can reapply and receive IDAPE payouts again if your loved one is assessed to meet all the eligibility criteria.
To change scheme details
Log in with Singpass on eFASS. Go to “Manage My Schemes” > “Change in Scheme Details.”
If you are updating the details for someone who lacks mental capacity for the first time, please read here.
To change the payee to a nursing home that the care recipient is living at
If you are using the IDAPE to offset the cost of the nursing home fees, you can ask for the payout to be made directly to the nursing home.
For this change in payee, please approach the nursing home your loved one is residing at to help you submit the “Change in Application Details” Form to AIC.
Do keep a copy of the application documents for your own reference.
To stop receiving payouts
Log in with Singpass on eFASS. Go to “Manage My Schemes” > “Change in Scheme Details.”
If you are unable to do any of the above online, email apply@aic.sg to obtain a copy of the application form or visit any AIC Link. We seek your understanding that hardcopy applications will require a longer approval waiting time.
No. IDAPE’s eligibility criteria are stricter as it is a severe disability scheme.
If your loved one is eligible for IDAPE, you can automatically receive PioneerDAS or HCG payouts without going for a separate assessment (if you meet those schemes’ criteria), but not the other way around.
To be eligible for IDAPE, the care recipient must not be a policyholder of CareShield Life, ElderShield and/ or its supplement plans.
Also, the care recipient would not be eligible for IDAPE if any claims related to CareShield Life, ElderShield, CareShield Life or ElderShield supplement plans have been made.
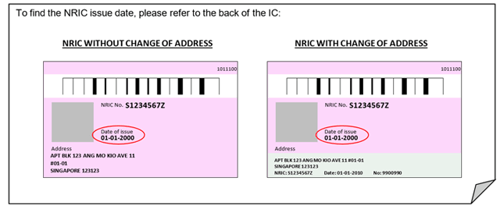
AIC needs the NRIC issue date for verification. You can find it on the back of your NRIC card.
Visit SG Enable’s Enabling Guide, an online resource for persons with disabilities and their caregivers, as well as professionals looking for disability support.

